Part 1 of 2.
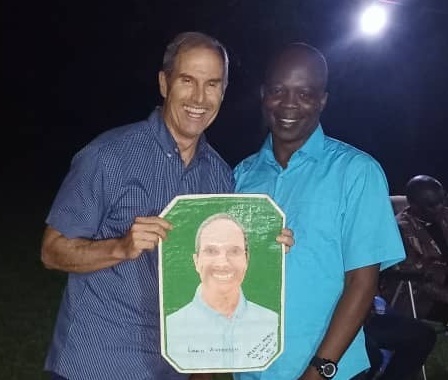
Dr. Jim Walker, PCP Medical Ambassador
The word that most often comes to my mind about the medical situation in Congo is incomprehensible. When I first became a Medical Ambassador four years ago, I learned that one in five children in the Democratic Republic of Congo die by age five, and that Congo was the most dangerous place in the world to deliver a baby. Last year I asked how many clinics had both a blood pressure cuff and stethoscope—only about two-thirds did. During a previous trip, all twelve of the doctors and nurses knew of a patient who had a leg paralyzed from an injection. On my recent trip in September 2017, as I was reteaching Managing Bleeding After Birth, one of the providers asked whether if while waiting three minutes to clamp the cord he should just put the baby on the mothers chest to keep it warm. Another quick survey revealed only seven of the twenty nurses knew how to resuscitate a baby. Suddenly, I was also reteaching newborn resuscitation. I was thankful I was able to teach resuscitation where, unfortunately, babies did not survive unless healthcare workers had the resources and training to resuscitate non-breathing babies. The next morning, one of the nurses said she attended a birth during the night and the baby was not breathing. She suctioned and bagged the baby as trained, and it was alive and well. That was a definite highlight!
To address these issues, an organization called Jhpiego (a nonprofit affiliated with Johns Hopkins University) has developed a curriculum called Saving Lives at Birth, which is a training program designed to build the capacity of health workers all over the world who provide care for women and newborns at birth. Four years ago, Dr. Eric Gunnoe taught the course Helping Babies Breathe at the request of Congolese nurses, so they could learn how to resuscitate non-breathing newborns. Since then, PCP has provided newborn resuscitation equipment for all the hospitals and clinics supported by the Covenant Church of Congo. My teaching focus has been on saving the lives of mothers. In my two previous trips, I taught Helping Mothers Survive: Bleeding After Birth, which is designed to help prevent maternal bleeding. This past September, my primary goal was to teach a new course on managing blood pressure in pregnancy, called Helping Mothers Survive: Blood Pressure in Pregnancy (Pre-eclampsia & Eclampsia).
The best thing about traveling to Congo as a Medical Ambassador is developing relationships with the doctors and nurses that we interact with and teach. I knew one-third of the 23 doctors and nurses in this training from previous trips. They are very good students, especially good at oral learning. The goal of the Train-the-Trainer approach is to enable our students to teach other Congolese health professionals. To that end, we bring in students from the nursing schools in Karawa and observe them teaching the course they have just taken. One of the nurses succinctly taught the entire course only three days after she had first learned all the material. All the doctors and nurses collaborated in the teaching. Dr. Nathan Stockcamp, who joined us for the week, teaches graduate-level physicians in the U.S. He told the Congolese students that how they learned and presented the material exceeded what he could have expected from his own students.
Easily the most fun part of the course is when our students strap on the Mama Natalie baby doll mannequins and simulate labor and delivery. Dr Eric was initially concerned that the male Congolese doctors and nurses would not like simulating a woman in labor. Wrong. Both men and women love pretending to be a laboring woman. The environment is raucous, but also much is learned.
What I liked most about this trip was being part of a teaching team. Marta Klein translated the information into Lingala, interjecting information from her experiences in Congo. Ann Hagensen and my daughter, Julie Malyon, taught a nursing skills lab that included taking blood pressure, medication dilution, and injection techniques. Sheryl Noren’s preparatory work made the teaching possible. The culmination of the class is the awarding of certificates of course completion, and the Congolese nurses love this part!
So will this training make a difference? I am optimistic that as the Congolese health care providers utilize the Train-the-Trainer approach to disperse this knowledge throughout the area, the lives of mothers and newborns will be saved.
If you or someone you know is interested in the Medical Ambassador Program, please contact us today! Or, consider donating to our Medical Ambassador trips to Congo so we can continue this life-saving training program. Thank you!
Coming up: Dr. Gado, CEUM Medical Director, reports on the Pre-Eclampsia/Eclampsia training in Karawa.